May 18, 2020
The issuance of the 1135 waiver permits the Medicare program to cover visits, pharmacologic management, individual psychotherapy, and other professional services furnished to (and from) any location in the country – including the patient’s place of residence. In other words, CMS has removed all Medicare telehealth originating site requirements. Additionally, CMS has also relaxed restrictions on the types of telecommunications devices eligible to perform telehealth. Medicare now covers telehealth services performed using any device which offers real-time communication with audio and video. Notably, this includes devices not generally considered HIPAA compliant. Therefore, during this public health emergency, Medicare telehealth services may be performed using cellular telephones, tablets, and/or computers using applications such as FaceTime or Skype. In accordance with this policy, the Department of Health and Human Services (HHS) Office for Civil Rights (OCR) is exercising enforcement discretion and waiving penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies during the COVID-19 nationwide public health emergency. For more information on HIPAA enforcement, please visit: www.hhs.gov/hipaa/forprofessionals/specialtopics/emergencypreparedness/index.html.
A complete list of all Medicare telehealth services can be found here: https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes.
CMS has explained telehealth services performed under these waivers will be paid under the Physician Fee Schedule at the same amount as in-person services. In order to receive full payment, however, clinicians must bill the service using the place of service (POS) code representing their normal practice location (i.e. office). The clinician will then append modifier 95 to indicate the service was furnished by telehealth. There is no requirement to enroll a new practice location, including a clinician’s home address, despite the fact they may be located there when the service is performed. Nevertheless, any claims submitted with a clinician’s home address, or other physical location, should still be paid.
Traditional telehealth services may also be billed during this time. In those cases, the clinician at the distant site would bill using the POS 02, to indicate the service was performed via telehealth. Per usual, coding in this manner will result in a payment at the lower facility rate, as it takes into account a qualified originating site also billing for the service. CMS anticipates most telehealth services will not be billed in the traditional manner during this emergency period. We have attached another fact sheet detailing the Medicare telehealth policy.
COVID-19 FAQs on Medicare Fee-for-Service Billing.
https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf
April 7, 2020
UPDATE
News
Billing for Professional Telehealth Distant Site Services During the Public Health Emergency — Revised
This corrects a prior message that appeared in our March 31, 2020 Special Edition.
Building on prior action to expand reimbursement for telehealth services to Medicare beneficiaries, CMS will now allow for more than 80 additional services to be furnished via telehealth. When billing professional claims for all telehealth services with dates of services on or after March 1, 2020, and for the duration of the Public Health Emergency (PHE), bill with:
· Place of Service (POS) equal to what it would have been had the service been furnished in-person (see grid below)
· Modifier 95, indicating that the service rendered was actually performed via telehealth
As a reminder, CMS is not requiring the CR modifier on telehealth services. However, consistent with current rules for telehealth services, there are two scenarios where modifiers are required on Medicare telehealth professional claims:
· Furnished as part of a federal telemedicine demonstration project in Alaska and Hawaii using asynchronous (store and forward) technology, use GQ modifier
· Furnished for diagnosis and treatment of an acute stroke, use G0 modifier
|
Place of Service Code(s) |
Place of Service Name |
Place of Service Description |
|
11 |
Office |
Location, other than a hospital, skilled nursing facility (SNF), military treatment facility, community health center, State or local public health clinic, or intermediate care facility (ICF), where the health professional routinely provides health examinations, diagnosis, and treatment of illness or injury on an ambulatory basis. |
April 3, 2020
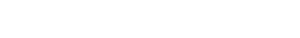
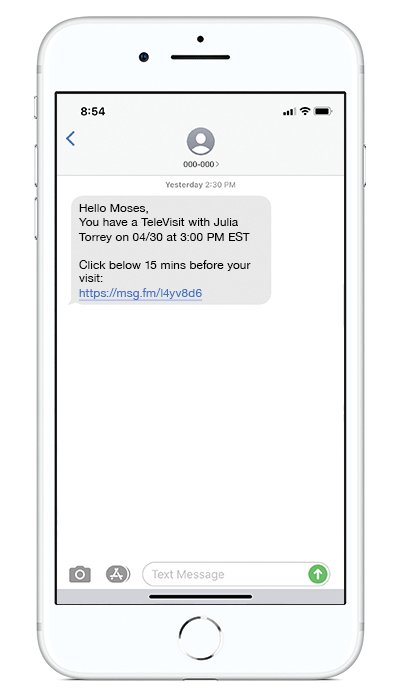
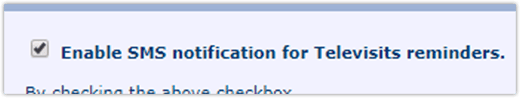
ECW USERS New feature announcement for healow TeleVisits
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
March 27, 2020
At the link here, it talks specifically about the 3 different types of visits covered under the telehealth waiver, and at the very bottom gives a break down of codes to use for each.
https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
From the FAQ, which I have attached, here is the language regarding the modifiers:
18. Q: Will CMS require specific modifiers to be applied to the existing codes?
A: CMS is not requiring additional or different modifiers associated with telehealth services furnished under these waivers. However, consistent with current rules, there are three scenarios where modifiers are required on Medicare telehealth claims. In cases when a telehealth service is furnished via asynchronous (store and forward) technology as part of a federal telemedicine demonstration project in Alaska and Hawaii, the GQ modifier is required. When a telehealth service is billed under CAH Method II, the GT modifier is required. Finally, when telehealth service is furnished for purposes of diagnosis and treatment of an acute stroke, the G0 modifier is required.
Below are the 2020 Telehealth Codes and Frequesntly asked questions from the following website:
https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes
Telehealth Codes Medicare Telehealth FAQs
Please Note that this is some information we have complied, it may have updates as of today. We will try to check for updates and send them post the periodically.
Payor Telehealth Waiver
|
List of Telehealth Services | CMS List of services payable under the Medicare Physician Fee Schedule when furnished via telehealth. Covered Telehealth Services CY 2019 and CY 2020 (Updated 11/01/19) (ZIP) |